An aging population, soaring rates of diabetes linked to growing obesity, and a rise in people with autoimmune diseases – these factors help to explain why more people are living with chronic wounds. Non-healing wounds are not just painful and debilitating; they are the lead cause of amputation and can sometimes prove fatal.
The key to finding effective therapies lies in understanding the complex interplay between cells and molecules that determine whether a skin wound heals normally or becomes chronic. But treatment has been held back by a lack of research in this area and huge gaps in our knowledge about wound repair.
Most skin wounds follow a straightforward sequence of healing: some cells act to prevent infection, others to stop the bleeding and repair the wound. The inflammatory response needs to be sufficient to control infection while avoiding damage to host tissues. Current knowledge suggests that a wound can become chronic by being ‘stuck’ in its inflamed state, which stops it from healing properly. But why and how does this happen?
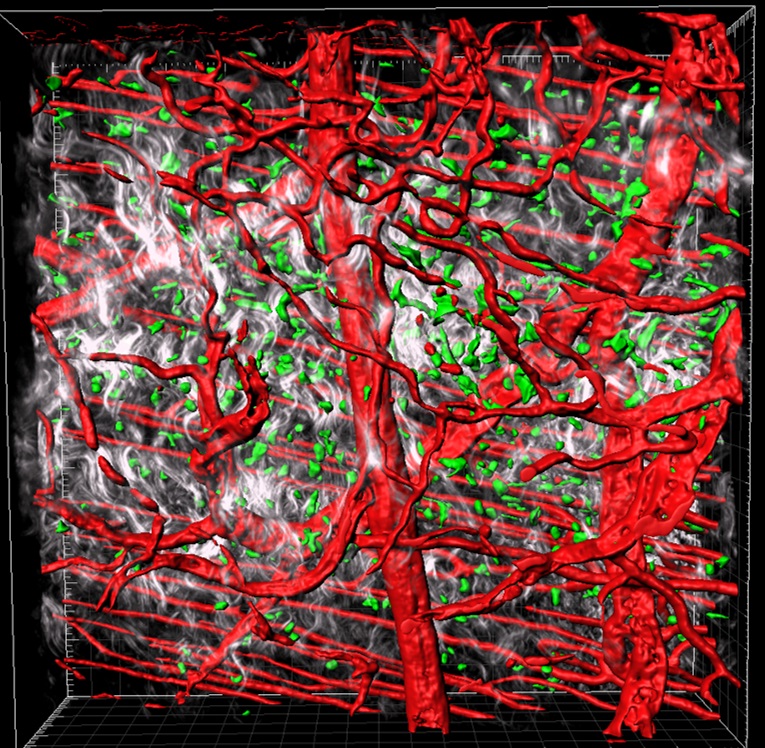
Dr Cash used the EBI Early Career Fellowship to establish a clinically relevant mouse model of human chronic wounds and a novel imaging technique for ‘live’ observation of skin repair in a mouse. Crucial to this work was a new, state-of-the-art, multiphoton microscope in the Wolfson Bioimaging Facility.
Dr Cash also benefitted from two academic mentors in the School of Physiology, Pharmacology and Neuroscience: Professor Paul Martin, internationally renowned for his animal studies of cancer and wound repair; and Professor Alastair Poole, a world leader in platelet biology.
Dr Cash first became interested in wound repair as a postdoctoral research fellow, when she patented a chemerin peptide (C15) that accelerated skin repair and reduced scarring by inhibiting immune cell responses in inflammation. This was her first collaboration with Professor Martin; other collaborators were Professor Mauro Perretti (William Harvey Research Institute, London) and Professor Paul Kubes (Calgary University, Canada).
The publication of this work allowed her to gather preliminary data for further grant applications to establish her own independent research group. She ultimately secured a Chancellor’s Fellowship (University of Edinburgh) and has since been awarded £1.157 million from the Wellcome Trust and Royal Society and the Chancellors Fellowship which provided start -up costs and funding for a PhD student.
This prestigious Sir Henry Dale Fellowship enabled her to establish her own lab at Edinburgh’s MRC Centre for Inflammation Research under the mentorship of Prof Moira Whyte (head of CIR and the College of Medicine and Veterinary Medicine) and Prof Stuart Forbes (head of MRC Scottish Centre for Regenerative Medicine).
Her research is aiming to reveal the role of macrophages (white blood cells) in normal wound repair and in non-healing chronic wounds. Dr Cash has since established a human chronic wound database in collaboration with the NHS Lothian Tissue Bank.
