CTB group
 Colorectal Tumour Biology Group
Colorectal Tumour Biology Group
Colorectal tumour cell survival mechanisms and chemoprevention
Current research aims:
- Discovering novel context-dependent targets for β-catenin: exploiting the tumour microenvironment for chemoprevention.
- Unravelling the regulation of PGE2 metabolism: can we target the earliest events in colorectal carcinogenesis?
- Identifying whether the function of BAG-1 as a regulator of transcription can explain its oncogenic role in colorectal tumorigenesis?
- Studying the biology of intestinal stem cells to identify novel targets for therapeuitc intervention.
- Translational Research: we have a major commitment to translate our basic research to the clinic and have been principal investigators in establishing both local and national clinical trials.
Background and Research Plan:
Colorectal cancer remains the second most common cause of cancer death in the UK and epidemiological evidence suggests that between 50-80% are preventable. Chemoprevention (primary and secondary) provides one of the greatest opportunities to impact significantly on this disease. Thus, there is an urgent need to develop novel preventive and therapeutic strategies for colorectal cancer.
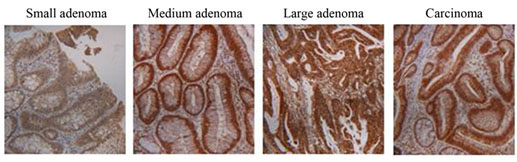
Colorectal cancer is an excellent example of the complex multistage process of carcinogenesis. Most colorectal cancers develop from adenomas (benign tumours also called polyps) in what is often referred to as the adenoma-carcinoma sequence. One of the key pathways regulating intestinal homeostasis is the wnt pathway; deregulation leading to increased β-catenin signalling is believed to be one of the earliest events in colorectal carcinogenesis. In addition, progression of small adenomas to large highly dysplastic adenomas before they ultimately develop into carcinomas is associated with high expression of the cyclooxygenase enzyme COX-2, leading to increased prostaglandin production; PGE2 having been shown to play a major role in promoting tumour cell growth. Our laboratory has a long standing interest in colorectal tumour biology and more recently the cross-talk between the wnt and COX-2/PGE2 signalling pathways and colon cancer stem cell biology.
The progression of colorectal cancer via the pre-malignant adenoma offers a number of potential stages and targets for chemoprevention, and in this context we have a long standing interest in the action of non-steroidal anti-inflammatory drugs [NSAIDs] such as aspirin, known to inhibit the COX/PGE2 signalling. Targeting the COX/PGE2 signalling pathway has been, and promises to be, one of the most successful approaches to prevent bowel cancer. For this reason there remains considerable interest in understanding the tumour promoting effects of PGE2, which is known to influence most, if not all, of the hallmarks of cancer [Greenhough et al., Carcinogenesis 2009]. Firstly, to increase our understanding of fundamental mechanisms of tumorigenesis, and secondly to discover novel targets for chemoprevention. Moreover, there is continuing interest in the use of non-selective and COX-2-selective NSAIDs for chemoprevention in individuals at high risk of developing cancer and as adjuvants to therapy.
As well as key genetic and epigenetic events that drive colorectal tumorigenesis, recent studies highlight the importance of the tumour microenvironment not only in tumour development and progression but also in the tumour response to chemopreventive/therapeutic agents. In fact, there is evidence that metabolic stress occurs during the premalignant stages of tumorigenesis as well as in cancers, leading to significant interest in targeting the tumour microenvironment both for chemoprevention and therapy. Recent findings unveiled a completely new role for β-catenin during colorectal tumorigenesis mediating adaptation to hypoxia, as summarised below.

Under normoxic conditions, COX-2 expression can be induced through the activation of oncogenic pathways such as the Ras-MAPK pathway. Furthermore, COX-2-derived PGE2 promotes cell proliferation at least in part via the stimulation of β-catenin/TCF-4 activity, as well as via enhancement of Ras-MAPK signalling. During hypoxia, β-catenin is displaced from TCF-4 (which results in TCF-4 repression) via its interaction with HIF-1, and β-catenin enhances HIF-1 transcriptional activity. In addition, COX-2 is up-regulated during hypoxia via HIF-1 activation, resulting in increased levels of PGE2. Both enhanced HIF-1 transcriptional activity and increased PGE2 levels promote cell survival leading to adaptation to hypoxia. Whereas β-catenin acts as essential activator of TCF-4 in normoxia, β-catenin results in the enhancement of HIF-1 transcriptional activity during hypoxia. These effects are likely to be transient and reversible (dynamic) depending on the tumour microenvironment and fluctuations in oxygen levels [Kaidi et al., Nature Cell Biol 2007].
Dynamism in transcription factor function in response to microenvironmental stress provides new avenues for selective targeting of tumour cells and in this context we have made the potentially exciting observation that BAG-1 is a potentiator of NF-κB function (Clemo et al., Carcinogenesis 2008). We first identified BAG-1 as an important protein in colorectal carcinogenesis through its interaction with the tumour suppressor gene pRb (Arhel et al., Int. J. Cancer 2003). Since then we have shown that this interaction is important in determining the nuclear localisation and function of BAG-1 in colorectal tumour cells. BAG-1 is a multi-functional protein that exists in three major isoforms generated from a single mRNA via alternate initiation of translation. Although established as a HSP70/HSC70 co-chaperone, the function of nuclear localised BAG-1 protein is not well understood. Currently we are focusing on the role of BAG-1 in regulating transcription, it’s interaction with the COX-2/PGE2 axis and whether, through activation or repression of target genes, BAG-1 promotes tumour cell survival in the context of the tumour microenvironment.
We are currently involved in translational studies investigating the potential of prostaglandins as biomarkers for colorectal cancer and the use of NSAIDs as adjuvants in pre-operative therapy for rectal cancer.
