

Investigators and Projects
The complement system is a central component of innate immunity, consisting of a large family of plasma and membrane bound proteins that are critical for protection against bacterial infection and immune complex deposition. More recently, it has also been found to be functional in adaptive immune responses, with roles identified in antigen processing and presentation, T-cell proliferation and differentiation, and systemic tolerance. In organ specific autoimmune disease, inappropriate activation of the complement system amplifies the pathology of human and/or experimental diseases, including rheumatoid arthritis, multiple sclerosis, and macular degeneration. Complement activation exerts harmful effects through the generation of complement protein cleavage products, which promote and perpetuate inflammatory reactions.
Activation of complement occurs during the development and progression of several immune mediated ocular conditions including age-related macular degeneration (AMD) and uveitis, as well as neuro-retinal degenerative disorders. The cleavage of C5 into fragments C5a and C5b is a critical event during the complement cascade, as C5a is a potent pro-inflammatory anaphylatoxin capable of inducing cell migration, adhesion and cytokine release, whilst the membrane attack complex C5b-9 causes cell lysis. Therapeutic approaches to prevent complement induced inflammation include the use of blocking monoclonal antibodies (mAb) to prevent C5 cleavage.
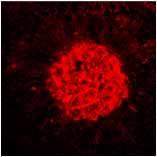
Work from the lab has examined the effect of inhibiting the C5 cleavage in terms of disease progression and severity in EAU, a model of organ-specific autoimmunity in the eye characterized by structural retinal damage mediated by infiltrating macrophages. Systemic treatment with a C5 blocking mAb, results in significantly reduced disease scores as compared with control groups, and local administration results in an earlier resolution of disease. In vitro studies have demonstrated that contemporaneous C5a and IFNgamma signaling can enhance nitric oxide production, and this is accompanied by down-regulation of the inhibitory myeloid CD200 receptor. Collectively, the data demonstrates that C5 cleavage contributes to the full expression of EAU, and that selective C5 blockade via systemic and local routes of administration can suppress disease. This presents great therapeutic potential to protect against tissue damage during autoimmune responses in the retina.
Complement and macrophage activation is also important in the development of choroidal neovascularisation (CNV), a signature of the wet form of AMD. Ongoing studies are examining the role of macrophages during the development of CNV. Utilizing the established laser-induced CNV model, in which laser-induced disruption of retinal pigment epithelium (RPE) and Bruch’s membrane causes an early inflammatory response including complement activation, followed by macrophage recruitment and VEGF up-regulation. Results indicate that early infiltrating macrophages possess a proangiogenic phenotype prior to CNV formation. Inhibiting complement activation through C5 blockade reduces macrophage infiltrate and VEGF expression, with a resultant suppression of CNV. The data suggests that control of macrophage activation is governed by the extent of RPE damage, leading to a proangiogenic macrophage phenotype, and the development of CNV resembling that seen clinically during the evolution of CNV in AMD.
D. A. Copland, K. Hussain, S. Baalasubramanian, T. R. Hughes, B. P. Morgan, H.
Xu, A. D. Dick and L. B. Nicholson (2010) Systemic and local anti-C5 therapy
reduces the disease severity in experimental autoimmune uveoretinitis
Clin. Exp. Immunol. 159: 303-314